If colleges billed their students at the end of four years and didn’t show us prices beforehand, it would wreck mass chaos. Or if airlines billed us at the end of flights and did not show us prices, it would lead to unstable markets. Both cases would enable price gouging and ultimately pricing failure. Our healthcare is designed around a similar consumerist regime and a global pandemic exposes the inequities of our healthcare system.
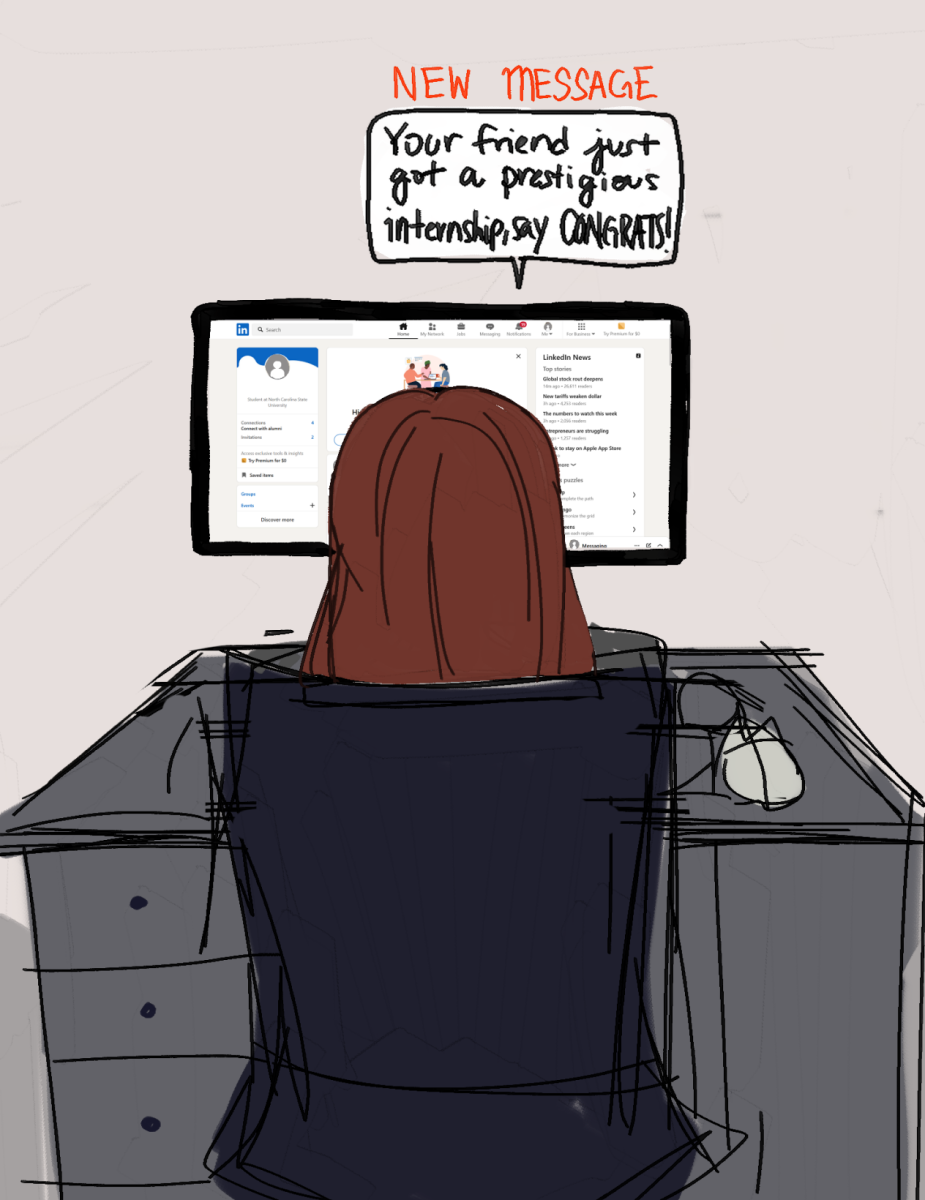
Before the pandemic, ‘pharmacy benefit managers,’ middlemen non-existent in other successful healthcare systems, led to overcharging of patients. Americans with chronic, unforeseen diseases have their entire lives disrupted with bad credit imposed by a system that is not affordable.The stakeholders are insurance companies, drug and device manufacturers making record-high profits off the backs of workers with health insurance, often by hitting them with surprise and inflated bills.
However, our quality of care is still unparalleled but even healthcare workers cannot justify or interpret the bills issued to their most vulnerable patients. Dr. Marty Makary, a cancer surgeon and professor of health policy at Johns Hopkins University is best known for two of his initiatives, the first being Restoringmedicine.org, which consists of tips for negotiating medical bills and provides advocacy work for public accountability around hospital bills. The second is Improving Wisely, a Robert Wood Johnson Foundation project aiming to lower health costs.
Closer to home, NC State has put together its most distinguished faculty as a COVID-19 Response team. Dr. Julie Swann, part of this team, was on loan as a science advisor for the H1N1 pandemic response at the Centers for Disease Control and Prevention. Swann’s past research includes the spread of influenza pandemics and access to health care drawing similar conclusions.
During the pandemic, Americans face higher out-of-pocket costs for their medical care than citizens of almost any other country, and research shows people forgo care they need, including for serious conditions, because of the cost barriers. The weaknesses in this system, which already puts the US behind its peers on so many health counts, are laid bare in an outbreak.
Universal health care is also not a perfect treatment for a pandemic, but it is a much better solution, more centralized planning is an asset in this crisis. Crafting a rapid, centralised response will have three key benefits, increase in response efficacy, improvement in quality of information and in response agility. The idea of ‘nerve centers’ has been thrown around, they coordinate activities across areas of responsibilities, such as communication, labor, economic development, education, energy, transport and most importantly medical response. Instead, we have adapted with a temporary patch on major structural problems.
It is extremely important where we go from here, after the pandemic, the healthcare system is no longer like the weather, we cannot simply discuss it and move on. To prevent future pandemics, Bill Gates has been warning us of the dangers of a disease outbreak for decades now, and has suggested that we adopt a data surveillance system that would instantly give relevant organizations the information they need about potential outbreaks. Taiwan has a similar system and has record low cases of COVID-19. At this point of time, the healthcare system is humanity’s biggest crutch with our existence hinging upon it. Decommercializing the system with more affordability and ease of access is the key to our broken system. The price we pay right now is way too high.